When trainees are exposed to patients who recover from a substance use disorder, it is humanizing, destigmatizing, and unforgettable, said Shelly F. Greenfield, M.D., M.P.H., a member of APA’s Council on Addiction Psychiatry, at the virtual meeting of the American Association of Directors of Psychiatric Residency Training (AADPRT).

“When trainees have that opportunity to work with a patient with a substance use disorder over time and see the patient get better in a real-world setting, it is incredibly gratifying,” says Shelly F. Greenfield, M.D., M.P.H.
Residents and fellows need more of those experiences. Greenfield cited data from surveys of program directors and from an October 2020 APA Resource Document on Education and Training for Substance Use Disorders (see section below) indicating that trainees generally do not receive sufficient training in the treatment of substance use disorders (SUDs), including faculty supervision focused specifically on treatment of SUD patients over time. Additionally, too few residents receive training in prescribing buprenorphine and other medications approved for treating SUDs.
“When trainees graduate as early career psychiatrists—no matter where they practice—they will see a very high proportion of patients with an SUD either alone or co-occurring with another psychiatric disorder,” Greenfield said. “Yet they have very little training in their four years overall. There have been some positive changes in addiction training in residency, but most studies and the APA resource document demonstrate that training for diagnosing and treating patients with substance use disorders is inadequate for graduating residents in 2021.”

Discover The World's MOST COMPREHENSIVE Mental Health Assessment Platform
Efficiently assess your patients for 80+ possible conditions with a single dynamic, intuitive mental health assessment. As low as $12 per patient per year.
She noted that the requirement of the Accreditation Council for Graduate Medical Education for just four weeks of dedicated training in addiction has not been changed since 2001. A 2012 survey of 104 program directors supported by the APA Council on Addiction Psychiatry found that only 19% of program directors reported that trainees were paired with supervisors for addiction, and 68% said patients with SUDs were sent elsewhere for treatment. Most did not provide opportunity for long-term treatment for patients with SUDs.
In comments to Psychiatric News after the meeting, Greenfield emphasized four areas in which training in addiction falls short:
-
Lack of supervision that is specifically focused on treatment of patients with SUD. Greenfield cited a 2018 survey of 84 program directors by the Addiction Task Force of AADPRT that found that in many programs addiction training takes place only on general psychiatry units in which co-occurring disorders are evaluated and treated, but the extent to which addiction-trained supervisors are available or addiction is the focus of the training is unclear. In that survey, 41.6% of program directors indicated there was a limited number of faculty with expertise in co-occurring conditions to provide trainee supervision.
Greenfield said one approach for programs that lack faculty expertise in addiction is collaboration with other programs, an opportunity made possible by the widespread use of video technology in medicine and psychiatry during the pandemic.
-
Failure to see patients over time. Trainees need to see the progress and recovery of patients with SUD over time. “Longitudinal experience with patients having SUD usually happens in outpatient settings where the trainee can treat patients with SUD, receive supervision, and be able to follow them beyond just a four-week experience on an inpatient unit,” Greenfield said.
-
Lack of training in using buprenorphine and other medications approved for addiction and SUD. “If residents have eight-hour waiver training in buprenorphine, they learn a lot about the medication and about opioid use disorder,” Greenfield said. “Data show that if you get just eight hours of training in residency, you are much more likely to prescribe this medication in your practice after residency. And yet we don’t have a requirement to complete that training.”
-
The tendency of residents to see patients with SUD only in the emergency department. “If you mostly expose trainees to patients who present to the emergency department with SUD, this can contribute to stigma and therapeutic nihilism—the belief that this condition never gets better,” Greenfield told Psychiatric News. “Most patients with SUDs are never seen in emergency departments.”
Psychiatrists should learn how to care for patients presenting in the emergency department with acute withdrawal or intoxication, she said, but most will graduate to practice in other settings—outpatient practices, community health settings, inpatient services, and residential and partial hospital settings. “Psychiatrists will routinely encounter patients in these settings who have substance use disorders including those with co-occurring psychiatric disorders, and it is imperative that they feel competent in providing that care.”
In addition to the APA resource document, Greenfield cited a number of resources for trainees and training programs. They include the Opioid Response Network and the Providers Clinical Support System, of which APA is a partner. This program offers training and mentoring in evidence-based prevention and treatment of opioid use disorders and treatment of chronic pain.
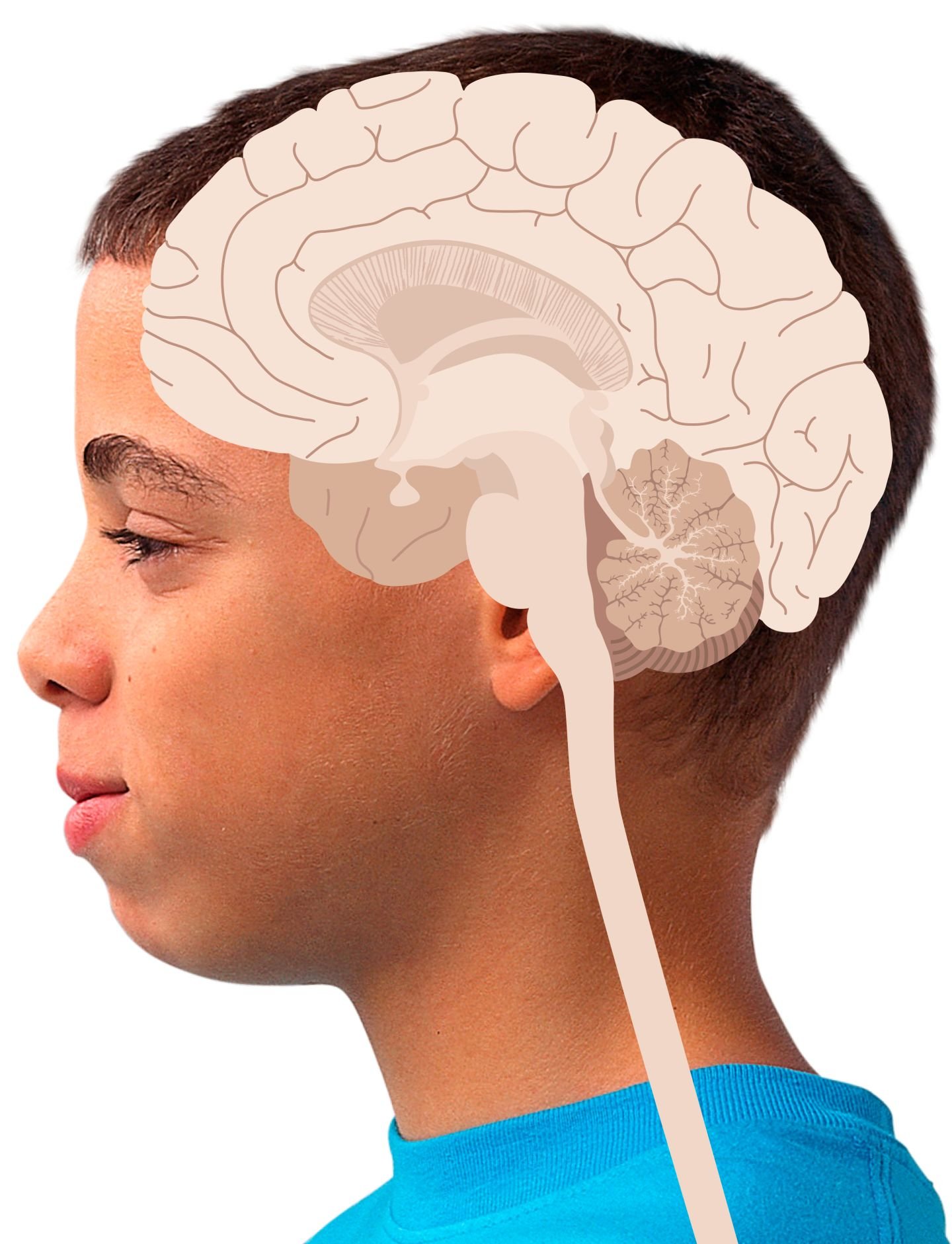
When trainees are expose to patients who recover from an SUD, it can be an experience the trainee will never forget.
“We have an apprentice system of learning in graduate medical education—as a resident you have a supervisor, but you are treating the patient yourself,” she said. “What we know is that when trainees have that opportunity to work with a patient with a substance use disorder over time and see the patient get better in a real-world setting—it’s incredibly gratifying.” ■
The APA Resource Document on Education and Training for Substance Use Disorders is posted here.
APA Resource Document Offers Recommendations for Medical Students, Residents, and Lifelong Learners
“Medical schools, physician training (residency) programs, and continuing education programs for physicians in practice provide limited training in the treatment of SUDs,” according to the APA Resource Document on Education and Training in Substance Use Disorders. “The scope of training on SUDs is disproportionate to the population health need to address these problems, and many with SUDs go undiagnosed and untreated.”
The resource document is a product of APA’s Council on Addiction Psychiatry, the Council on Medical Education and Lifelong Learning, and the Council on Healthcare Systems and Financing. The document offers recommendations for medical schools, residencies, and continuing medical education for physicians in practice, as well as strategies for change.
Recommendations for medical student rotations and residency programs include the following:
-
Addiction and co-occurring disorders should be incorporated into all aspects of psychiatry residency training since patients with SUD are seen at all levels of care.
-
Supervision and discussion of SUD cases should occur at inpatient and outpatient levels of care and should include an addiction psychiatrist.
-
Programs should ensure they have access to resources to help them incorporate enhanced training in SUD with the goal of bolstering resident competencies in assessing and treating patients for these conditions.
-
All psychiatry residents should complete the buprenorphine waiver training or its equivalent.
-
Residents should be trained to treat patients with alcohol use disorder, stimulant use disorder, opioid use disorder, sedative/hypnotic use disorder, cannabis use disorder, tobacco use disorder, and other substances.
-
Training experience should include various levels of patient acuity and corresponding care including outpatient and residential treatment.
-
Residents should receive training in the use of FDA-approved medications for opioid, alcohol, and tobacco use disorder (and others as developed and approved by the FDA).
-
Training on SUD treatments should include knowledge of the range of evidence-based behavioral therapies and competency to practice at least one. This might include, but is not limited to, the ability to integrate motivational interviewing concepts and techniques into patient assessments and sessions.
Source: https://psychnews.psychiatryonline.org/doi/10.1176/appi.pn.2021.5.23
Resource Document Calls for Improved Residency Training on SUDs | Psychiatric News